Living with inflammatory bowel disease (IBD) can be physically difficult and complex, especially if you have recently been diagnosed. Understanding the condition, its causes, symptoms, and available management strategies can help you better navigate daily life. Here is more information on IBD and useful insights for patients looking to learn more about IBD and its impact.
What Is IBD?
IBD is a chronic condition that causes inflammation in the digestive tract. It primarily includes two types of disorders: Crohn’s disease and ulcerative colitis. Crohn’s disease can affect any part of the gastrointestinal tract, while ulcerative colitis is confined to the colon and rectum. Though similar in some ways, these conditions differ in how they affect the digestive system.
The symptoms and severity of IBD can vary widely. While there is currently no cure, many treatment options are available to help manage symptoms and maintain quality of life. Consulting with a physician can help navigate avenues for treatment.
What Are the Causes and Symptoms?
The exact cause of IBD remains unknown, though research suggests several contributing factors. Genetics plays a key role, as patients with a family history of IBD are at a higher risk. Environmental triggers, such as diet and smoking, and an overactive immune response to gut bacteria are also thought to contribute.
Common symptoms of IBD include abdominal pain, diarrhea (sometimes with blood), fatigue, fever, the urgent need to have a bowel movement, and unintentional weight loss. Some individuals may experience flare-ups, where symptoms worsen, followed by periods of remission. Experiencing severe symptoms is a sign to talk to a doctor for help managing pain.
How Is It Diagnosed?
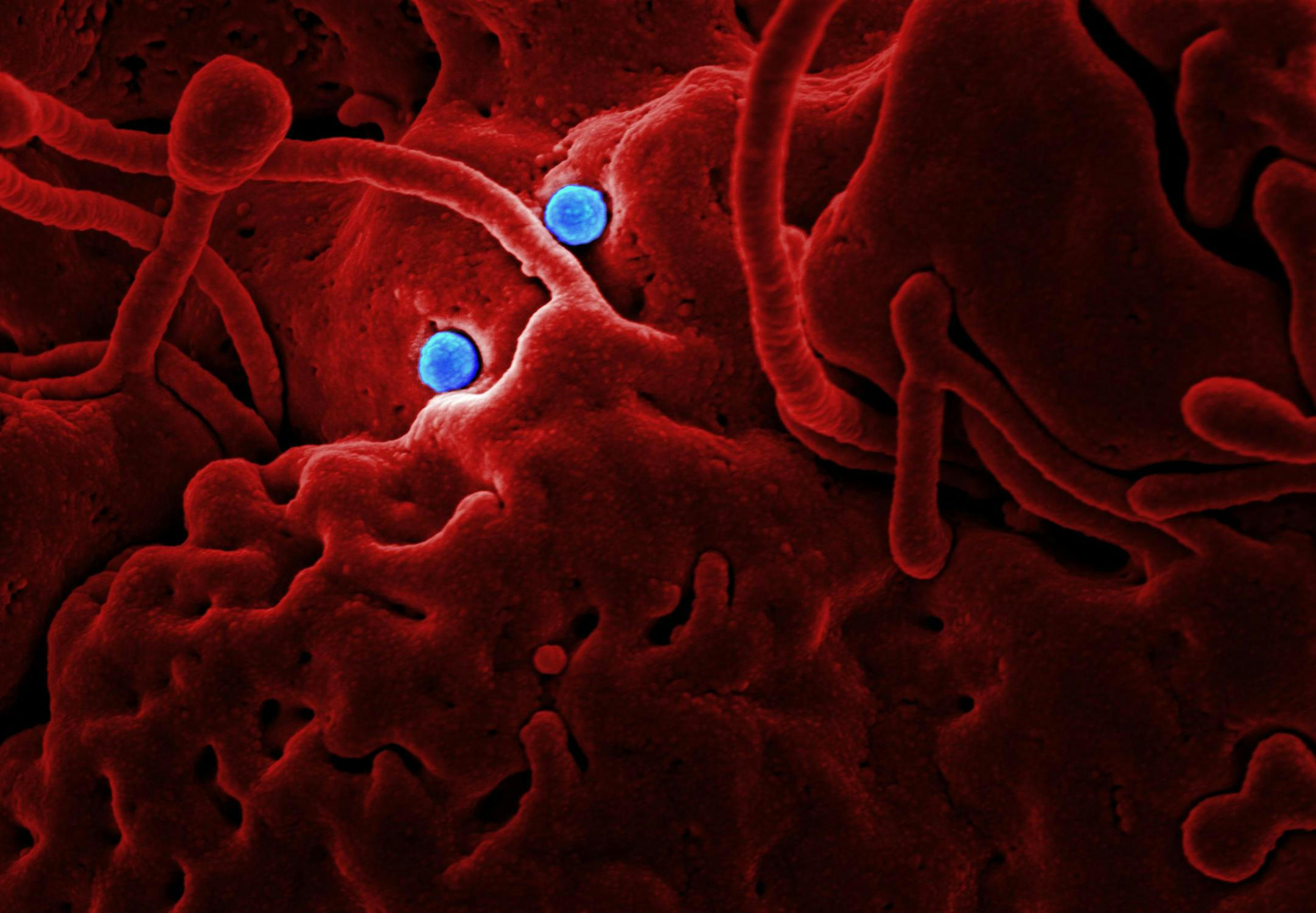
Diagnosing IBD typically requires a combination of approaches. A physician may begin with a detailed medical history and physical examination to assess symptoms and rule out other possible conditions. Blood tests and stool samples are often used to detect markers of inflammation or infection.
Further evaluation may involve imaging studies, such as CT scans or MRIs, to get a clearer look at the digestive tract. Endoscopic procedures, such as colonoscopy, allow doctors to examine the bowel lining directly and collect tissue samples for biopsy. An accurate diagnosis is helpful in developing an effective treatment plan.
How Can You Manage and Treat IBD?
Managing IBD often involves a combination of medication, dietary adjustments, and lifestyle changes. Medications can reduce inflammation, suppress the immune system, or address specific symptoms such as diarrhea or abdominal pain. For more severe cases, a surgical procedure to remove damaged portions of the GI tract may be recommended.
Diet and nutrition play a beneficial role in daily management. Nutritional counseling with a specialist may help manage painful symptoms and flare-ups. Lifestyle adjustments, including mental regulation, regular exercise, and stopping smoking, may also aid in managing symptoms. Regular follow-ups with your healthcare provider may be helpful to monitor disease progression and update your treatment plan as needed.
Learn More Today
Living with IBD comes with unique challenges, but understanding your condition is a beneficial first step. The right knowledge and management strategies can help you take control of your well-being. If you want to explore more about IBD and management options, consult with qualified healthcare professionals or explore additional educational resources. Taking the time to understand your diagnosis can pave the way for a more helpful approach to living with IBD.